Companion Guide
Background
FHIR stands for Fast Healthcare Interoperability Resources and was developed by HL7 (Health Level 7) to enable healthcare organizations to exchange information between different computer systems, regardless of how the data is stored in those systems. FHIR standards allow healthcare organizations to store and share patient data securely while ensuring interoperability between different systems by using a set standard. FHIR can be thought of as a common language that allows healthcare computer systems to communicate and exchange data using the internet, with the added benefit of being able to store the data in different ways. Healthcare organizations rely on FHIR standards to send information, including clinical and administrative data, for the benefit of patients receiving care. Using FHIR as a standard also allows for secure transmission of Personal Health Information, ensuring access to a patient’s data only when authorized.
Purpose
By setting a standard for health data formatting, FHIR facilitates the ability of healthcare organizations to develop an interface that can link to the internet and share health data using a common standard in real-time. The goal of FHIR is for healthcare organizations to be able to easily and securely share information using their existing Electronic Health Record systems, through the implementation of simple interfaces linked to the internet.
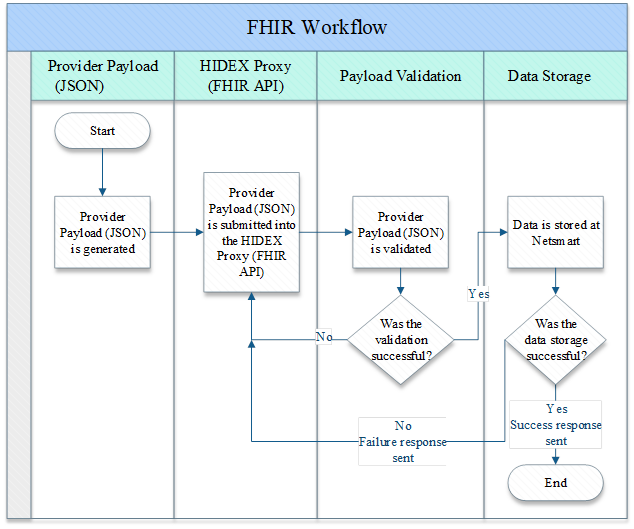
FHIR Workflow
FHIR Overview
The basis of HL7 FHIR are components called “Resources”. These “Resources” form the basic data exchange format and the model of FHIR. In FHIR, data is broken down into sections like patients, hospitals, or diagnostic results. Each of these sections are represented by a FHIR Resource which make an exchangeable patient record by defining the data elements, constraints, and relationships.
Each Resource has data elements that is necessary for its specific use case and connects relevant information with another Resource. For example, the Patient Resource has basic patient information such as name, gender, birthdate, along with contact information and it links with a Practitioner Resource which has information about the clinician nominated as the patient’s primary care provider. Resources use Uniform Resource Locators or URLs to be located within a FHIR system implementation
DPH SAPC uses Resources to connect workflows.
Each Resource has data elements that is necessary for its specific use case and connects relevant information with another Resource. For example, the Patient Resource has basic patient information such as name, gender, birthdate, along with contact information and it links with a Practitioner Resource which has information about the clinician nominated as the patient’s primary care provider. Resources use Uniform Resource Locators or URLs to be located within a FHIR system implementation
DPH SAPC uses Resources to connect workflows.
Core Resources
The following FHIR Resources under the FHIR R4 Standard will be supported in the HIDEX FHIR API.
| Fhir Resource | Version |
|---|---|
| Patient | v4 |
| Observation | v4 |
| EpisodeOfCare | v4 |
| Encounter | v4 |
| Condition | v4 |
| Coverage | v4 |
| QuestionnaireResponse | v4 |
Use Cases
The workflows identified and the subsequent Methods will be supported through the HIDEX FHIR API.
| Workflow | Fhir Resource | Method |
|---|---|---|
| Update Client Data | Patient | Put |
| Update Smoking Status | Observation | Get, Post, Put |
| Episode Search | EpisodeOfCare | Get |
| Diagnosis | Condition | Get, Post, Put |
| Women's Health History | Condition | Get, Post, Put |
| Financial Eligibility | Coverage | Get, Post, Put |
| Cal-OMS Admission | QuestionnaireResponse | Get, Post, Put |
| Cal-OMS Discharge | QuestionnaireResponse | Get, Post, Put |
Resources
Patient Resource
This resource covers data about patient involved in a wide range of health-related activities. This data covers the “Who” information of the patient. It focuses on the demographic information necessary to support the administrative, financial, and logistic procedures. The patient record is generally created and maintained by the organization providing care for the patient. If a patient is receiving care at multiple organization, they will have their information present in multiple Patient Resources. More information about the Organization Resource can be found in this website: https://hl7.org/fhir/R4/patient.html
Observation Resource
This resource covers data about patient's smoking status. Observations are a central element in healthcare, used to support diagnosis, monitor progress, determine baselines and patterns and even capture demographic characteristics. More information about the Observation Resource can be found in this website: https://hl7.org/fhir/R4/observation.html
Encounter Resource
The Encounter Resource is an interaction between a patient and healthcare provider(s) for the purpose of providing healthcare services(s) or assessing the health status of a patient. The patient resource is set apart by the setting in which it takes place. Examples include, ambulatory, emergency, inpatient, etc. An Encounter Resource encompasses the lifecycle from pre-admission to discharge. Due to the broad scope of Encounter, not all the data elements will be relevant in all settings. More information about the Encounter Resource can be found in this website: https://hl7.org/fhir/R4/encounter.html
Condition Resource
Condition is a clinical condition, problem, diagnosis or other event, situation, issue, or clinical concept that has risen to a level of concern. It is a clinician’s assessment and assertion of a particular aspect of a patient’s state of health. It can be for a diagnosis, a problem, or an ongoing health issue/concern. It could also be used to record a health state that is not normally a negative outcome, such as pregnancy. More information about the Condition Resource can be found in this website: https://hl7.org/fhir/R4/condition.html
Coverage Resource
Coverage includes insurance and self-payment, any financial instrument that can be used to reimburse or pay for health care products or services. This resource provides identifiers and descriptors of an insurance plan with information that would appear on an insurance card or when an individual has registered as “SelfPay” and is taking responsibility for payment of a portion of the healthcare costs. More information about the Coverage Resource can be found in this website: https://hl7.org/fhir/R4/coverage.html
QuestionnaireResponse Resources
The QuestionnaireResponse Resource is a structured set of questions and their answers. The questions are ordered and grouped into coherent subsets, corresponding to the structure of the grouping of the questionnaire being responded to. The responses cover the need to communicate data originating from forms used in medical history examinations, research questionnaires and sometimes clinical specialty records. More information about the QuestionnaireResponse Resource can be found in this website: https://hl7.org/fhir/R4/questionnaireresponse.html
Bundling Resources
A Bundle is a container for Resources. They enable Resources to be grouped and transmitted altogether at once. Resource Bundles are useful for a variety of reason some of which include
- Returning a set of resources that meet some criteria as part of a server operation
- Returning a set of versions of resources as part of the history operation on a server
- Sending a set of resources as part of a message exchange
- Grouping a self-contained set of resources to act as an exchangeable and persistable collection with clinical integrity
- Creating/updating/deleting a set of resources on a server as a single operation
- Storing a collection of resources
Hidex Onboarding
You will need to register your application with the Hidex Proxy at which point you will be issued a client Id and client secret. Your client id and client secret will be use to obtain an authentication token which will give you access to the HIDEX FHIR API endpoints.